Services
Your Health, Our Priority
Whether it’s pediatric care or orthopedic solutions, Dr. Vivek Shrivastava is committed to your well-being. Explore our comprehensive services, backed by years of experience and a passion for healing.
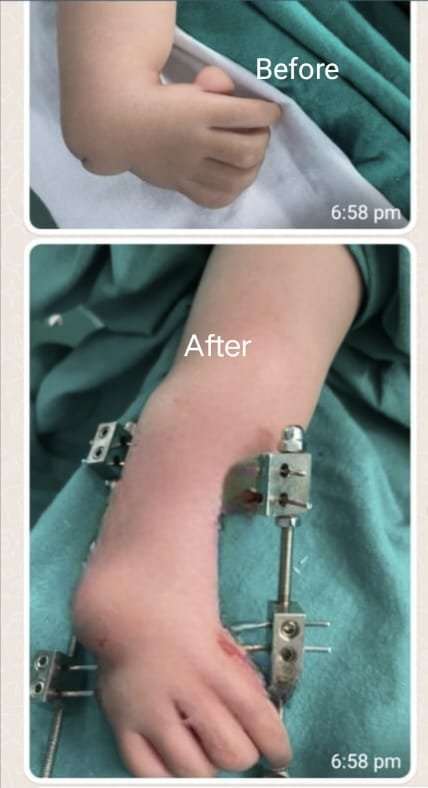
Radial Club Hand
Radial club hand, also known as radial deficiency, is a rare congenital condition that affects the development of the radius bone in the forearm. This results in a shortened or missing radius, leading to a curved or “club-like” appearance of the hand.
Some common characteristics of radial club hand include:
– Shortened or missing radius bone
– Curved or bent wrist and forearm
– Shortened or missing thumb
– Fusion or webbing of fingers
– Limited wrist and hand movement
Treatment options may include:
. Serial plaster to correct deformity
– Surgery to straighten the wrist and improve hand function
– Physical therapy to improve mobility and strength
– Orthotics or prosthetics to support hand function
– Occupational therapy to develop adaptive skills

Club Foot
Clubfoot, also known as talipes equinovarus, is a congenital deformity of the foot that affects approximately 1 in 1,000 births. Here’s an overview:
Causes and Risk Factors
1. Genetic predisposition
2. Environmental factors (e.g., intrauterine positioning)
3. Associated conditions (e.g., cerebral palsy, spina bifida)
4. Family history
Characteristics
1. Inward rotation of the heel (equinus)
2. Upward rotation of the foot (dorsiflexion)
3. Inward rotation of the ankle (varus)
4. Adduction of the forefoot (toe-in)
5. Rigidity and stiffness
Classification
1. Idiopathic (most common, 80-90%)
2. Neurogenic (associated with neurological conditions)
3. Syndromic (part of a larger genetic syndrome)
Treatment Options
Non-Surgical
1. Ponseti Method: Serial casting and manipulation (90-95% success rate)
2. Kite Method: Similar to Ponseti, with modifications
3. Physical therapy and bracing
Surgical
1. Posteromedial release surgery (PMRS): Release of tight tissues and tendons
2. Osteotomies: Cutting and realigning bones
3. Tendon transfers
Ponseti Method
1. Initial casting (1-2 weeks)
2. Weekly casting changes (4-6 weeks)
3. Achilles tendon tenotomy (if necessary)
4. Bracing (2-3 years)
Surgical Indications
1. Failed non-surgical treatment
2. Severe deformity
3. Older children or adults
4. Associated conditions (e.g., cerebral palsy)
Complications
1. Recurrence
2. Infection
3. Nerve damage
4. Limited mobility
Outcomes
1. Successful correction in 90-95% of cases
2. Improved mobility and function
3. Enhanced quality of life
4. Potential for long-term follow-up and management
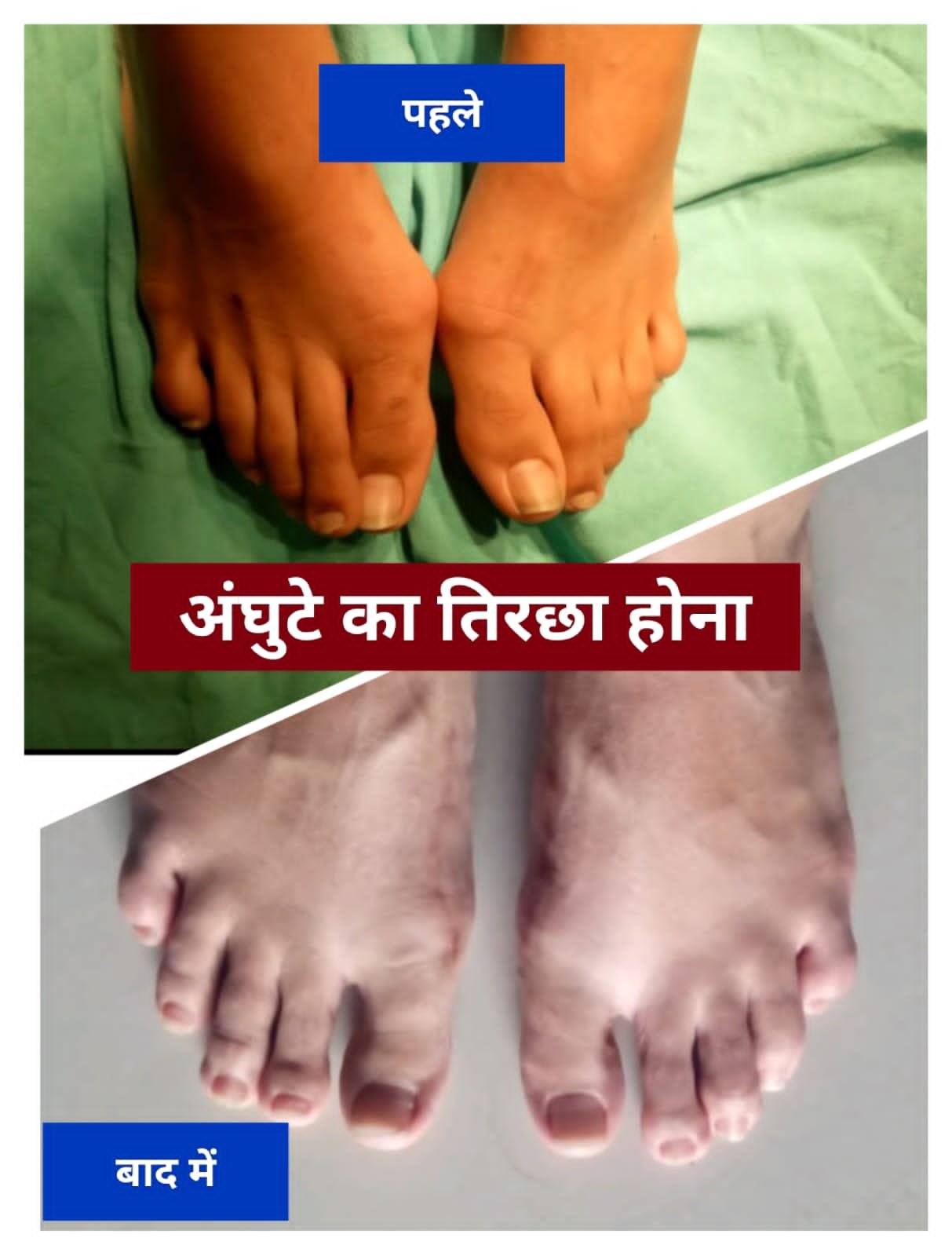
Foot Deformities
Any condition which alters the shape or structure of the foot into something painful or harmful.

Flat foot
If you see your child is walking with flat foot ,then child needs assessment to rule out condition in which bones of foot are not in proper alignment.

Vertical Talus
Congenital Vertical Talus (CVT), also known as Rocker Bottom Foot or Congenital Vertical Talus Deformity, is a rare congenital foot anomaly.
Incidence and Prevalence
1. Estimated 1 in 10,000 to 1 in 50,000 births
2. More common in males (2:1 ratio)
3. Bilateral involvement in 50-60% of cases
Causes and Risk Factors
1. Genetic predisposition
2. Chromosomal abnormalities (e.g., trisomy 13, 18)
3. Neural tube defects (e.g., spina bifida)
4. Intrauterine constraints or positioning
5. Family history
Characteristics
1. Vertical orientation of the talus bone
2. Dorsal dislocation of the navicular bone
3. Plantarflexion of the forefoot
4. Hindfoot equinus
5. Rigid or flexible deformity
Classification
1. Idiopathic (most common)
2. Neurogenic (associated with neurological conditions)
3. Syndromic (part of a larger genetic syndrome)
Diagnosis
1. Physical examination
2. Imaging studies:
– X-rays ( AP and lateral views)
– CT scans or MRI (for complex cases)
3. Differential diagnosis: other congenital foot deformities (e.g., clubfoot)
Treatment Options
Non-Surgical
1. Manipulation and casting (Ponseti method)
2. Physical therapy and bracing
3. Orthotics (e.g., ankle-foot orthoses)
Surgical
1. One-stage correction (dorsal opening wedge osteotomy)
2. Two-stage correction (initial casting, followed by surgery)
3. Osteotomies (e.g., calcaneal lengthening)
4. Tendon transfers or lengthening
Complications
1. Recurrence
2. Infection
3. Nerve damage
4. Limited mobility
5. Arthritis or degenerative changes
Outcomes
1. Successful correction in 80-90% of cases
2. Improved mobility and function
3. Enhanced quality of life
4. Potential for long-term follow-up and management
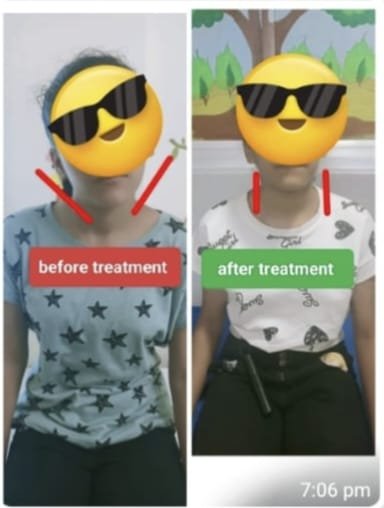
Torticollis
Torticollis, also known as wry neck, is a condition characterized by a twisted or tilted neck, resulting in an abnormal postural position. Here’s an overview:
Types:
1. Congenital Muscular Torticollis (CMT): Present at birth, caused by in-utero positioning or genetic factors.
2. Acquired Torticollis: Develops later in life due to various factors.
3. Spasmodic Torticollis: A neurological disorder causing involuntary muscle contractions.
Causes and Risk Factors:
1. Congenital factors (e.g., intrauterine positioning)
2. Genetic predisposition
3. Trauma or injury
4. Infections (e.g., mastoiditis)
5. Neurological conditions (e.g., cerebral palsy)
6. Musculoskeletal conditions (e.g., muscle imbalances)
Symptoms:
1. Twisted or tilted neck
2. Limited range of motion
3. Head tilt or rotation
4. Facial asymmetry
5. Pain or stiffness
6. Difficulty turning head
Diagnosis:
1. Physical examination
2. Imaging studies (e.g., X-rays, CT scans, MRI)
3. Electromyography (EMG) for spasmodic torticollis
Treatment Options:
Conservative:
1. Physical therapy (stretching, strengthening)
2. Occupational therapy (positioning, activities)
3. Orthotics (e.g., collars, splints)
4. Pain management (medications, injections)
Surgical:
1. Muscle lengthening or release
2. Tendon transfers
3. Osteotomies (bone realignment)
4. Spinal fusion (in severe cases)
Complications:
1. Permanent deformity
2. Chronic pain
3. Limited mobility
4. Facial asymmetry
5. Psychological impacts (e.g., self-esteem)

Polydactyly
Polydactyly of the foot, also known as extra toes, is a congenital anomaly characterized by the presence of additional toes.
Incidence:
1. Approximately 1 in 500 to 1 in 1,000 births
2. More common in males (2:1 ratio)
3. Bilateral involvement in 50-60% of cases
Types:
1. Postaxial polydactyly (most common): extra little toe
2. Preaxial polydactyly: extra big toe
3. Central polydactyly: extra toe in the middle of the foot
4. Polysyndactyly: extra toes webbed together
Causes and Risk Factors:
1. Genetic predisposition
2. Family history
3. Chromosomal abnormalities (e.g., trisomy 13)
4. Intrauterine constraints or positioning
5. Associated conditions (e.g., syndactyly, clubfoot)
Symptoms:
1. Visible extra toe(s)
2. Pain or discomfort
3. Difficulty fitting shoes
4. Cosmetic concerns
5. Potential for increased risk of ingrown toenails or other complications
Diagnosis:
1. Physical examination
2. Imaging studies (X-rays or CT scans)
3. Differential diagnosis: other foot anomalies (e.g., syndactyly)
Treatment Options:
Surgical:
1. Simple excision (removal of extra toe)
2. Reconstruction (realigning or recontouring surrounding tissues)
3. Osteotomy (cutting and realigning bones)
Non-Surgical:
1. Observation (monitoring for potential complications)
2. Orthotics (custom shoe inserts or braces)
3. Adaptive footwear
Complications:
1. Recurrence
2. Infection
3. Nerve damage
4. Limited mobility
5. Cosmetic concerns
Prognosis:
1. Excellent prognosis with prompt treatment
2. Improved function and cosmetics
3. Long-term follow-up for potential complications

Aneurysmal bone cysts
Aneurysmal Bone Cyst (ABC) is a rare, benign bone tumor that affects approximately 1.5 per 100,000 people.
Characteristics
1. Typically occurs in long bones (femur, tibia, humerus)
2. Expansile, blood-filled lesion
3. Multilocular, with fluid-filled cavities
4. Thin, fragile cortical bone
Causes and Risk Factors
1. Unknown etiology
2. Genetic predisposition
3. Trauma or injury
4. Association with other bone lesions (e.g., giant cell tumor)
5. More common in females (2:1 ratio)
6. Typically affects individuals between 10-30 years old
Symptoms
1. Pain (mild to severe)
2. Swelling or palpable mass
3. Limited mobility or stiffness
4. Pathological fracture (rare)
5. Neurological symptoms (if spinal involvement)
Diagnosis
1. Imaging studies:
– X-rays (radiolucent lesion with expansile margins)
– CT scans (multilocular, fluid-filled cavities)
– MRI (fluid-fluid levels, characteristic of ABC)
– Bone scan (increased uptake)
2. Biopsy (histological confirmation)
3. Differential diagnosis: other bone lesions (e.g., giant cell tumor, osteosarcoma)
Treatment Options
1. Surgical:
– Curettage (removal of lesion tissue)
– Bone grafting
– Internal fixation (if necessary)
2. Minimally invasive:
– Embolization (reduce blood flow)
– Radiofrequency ablation
3. Adjuvant therapies:
– Denosumab (anti-RANKL antibody)
– Bisphosphonates
Complications
1. Recurrence (10-30%)
2. Pathological fracture
3. Nerve or vascular damage
4. Infection
5. Malignant transformation (rare)
Prognosis
1. Excellent prognosis with prompt treatment
2. High recurrence rate requires long-term follow-up
3. Functional outcomes vary depending on location and extent of lesion
Radioulnar Synostosis
Radioulnar synostosis is a rare congenital or acquired condition where the radius and ulna bones in the forearm fuse together, limiting rotation and movement.
Types:
1. Congenital radioulnar synostosis (present at birth)
2. Acquired radioulnar synostosis (resulting from trauma, infection, or inflammatory conditions)
Causes and Risk Factors:
1. Genetic predisposition
2. Intrauterine constraints or positioning
3. Trauma or injury
4. Infection (e.g., osteomyelitis)
5. Inflammatory conditions (e.g., rheumatoid arthritis)
6. Associated conditions (e.g., clubfoot, cerebral palsy)
Symptoms:
1. Limited forearm rotation (pronation/supination)
2. Reduced elbow flexion/extension
3. Forearm deformity (e.g., valgus or varus)
4. Pain or discomfort
5. Decreased grip strength
Classification:
1. Proximal (near the elbow)
2. Distal (near the wrist)
3. Total (entire length of radius and ulna)
Diagnosis:
1. Physical examination
2. Imaging studies:
– X-rays (AP and lateral views)
– CT scans or MRI (for complex cases)
3. Differential diagnosis: other forearm conditions (e.g., Monteggia fracture)
Treatment Options:
Surgical:
1. Osteotomy (cutting and realigning bones)
2. Synostosis resection (removing fused bone)
3. Ulnar osteotomy (correcting ulnar deformity)
4. Radial head resection (in some cases)
Non-Surgical:
1. Physical therapy (improving range of motion)
2. Orthotics (forearm splints or braces)
3. Adaptive devices (e.g., adaptive utensils)
Complications:
1. Recurrence
2. Infection
3. Nerve damage
4. Limited mobility
5. Secondary conditions (e.g., osteoarthritis)
Prognosis:
1. Variable outcomes depending on severity and treatment
2. Improved function and mobility with surgical intervention
3. Long-term follow-up for potential complications

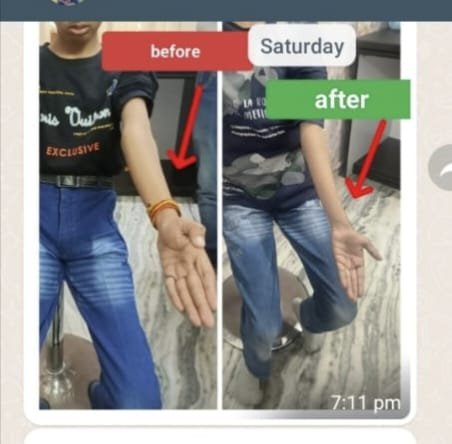
Humerus Varus Before
Child was unable to use his shoulder fully. Full range of movement after surgery.

Humerus Varus After
Child was unable to use his shoulder fully. Full range of movement after surgery.

Knock Knee
Knock knee, also known as genu valgus, is a condition where the knees touch or nearly touch each other, causing a gap between the ankles. It’s common in children and often corrects itself with growth.
Causes:
1. Genetic predisposition
2. Growth and development
3. Injury or trauma
4. Infections (e.g., osteomyelitis)
5. Neuromuscular disorders (e.g., cerebral palsy)
Symptoms:
1. Knees touch or nearly touch
2. Gap between ankles
3. Uneven gait or walking pattern
4. Difficulty standing or balancing
5. Pain or discomfort in knees, legs, or feet
Treatment:
1. Observation and monitoring
2. Bracing or orthotics
3. Physical therapy
4. Surgery (in severe cases)
Exercises to help correct knock knee:
1. Strengthening exercises (leg lifts, squats, lunges)
2. Stretching exercises (hamstring, quadriceps)
3. Balance and coordination exercises
When to seek medical attention:
1. Severe knock knee
2. Pain or discomfort
3. Difficulty walking
4. Uneven growth or development
5. Concerns about appearance or self-esteem

Knee Deformities Before
Genu valgum (knock-kneed): Head of tibia/fibula (not the joint itself), is inclined away from the midline of the body.

Knee Deformities After
Genu valgum (knock-kneed): Head of tibia/fibula (not the joint itself), is inclined away from the midline of the body.

Cerebral palsy
Orthopedic surgery is commonly performed in cerebral palsy (CP) patients to address musculoskeletal issues that affect mobility, posture, and overall quality of life.
Common Orthopedic Issues in CP Patients
1. Muscle spasticity and contractures
2. Hip subluxation or dislocation
3. Knee flexion or extension contractures
4. Foot deformities (e.g., equinus, varus, or valgus)
5. Scoliosis and other spinal deformities
6. Osteoporosis and fractures
Surgical Goals
1. Improve mobility and function
2. Enhance posture and balance
3. Reduce pain and discomfort
4. Prevent or correct deformities
5. Improve overall quality of life
Common Orthopedic Surgeries
1. Muscle lengthening procedures– Lengthening of muscles and tendons to reduce spasticity and contractures.
2. Tendon transfers– Transferring tendons to improve muscle balance and function.
3. Osteotomies– Cutting and realigning bones to correct deformities.
4. Hip reconstruction Surgery to correct hip subluxation or dislocation.
5. Spinal fusion Surgery to correct scoliosis or other spinal deformities.
6. Foot correction Surgery—to correct foot deformities.
7. Bone stabilization Surgery to stabilize bones and prevent fractures.
Considerations and Challenges
1. Complexity of CP- Each patient’s condition is unique, requiring individualized treatment plans.
2. Multiple surgeries- CP patients may require multiple surgeries throughout their lifetime.
3.Anesthesia risks- Patients with CP may have increased anesthesia risks due to associated medical conditions.
4. Postoperative care: Requires specialized rehabilitation and therapy to optimize outcomes.
5. Growth considerations– Surgeons must consider growth plates and potential impact on future growth.
Preoperative Evaluation
1. Comprehensive medical history and physical examination
2. Imaging studies (e.g., X-rays, CT scans, MRI)
3. Assessment of cognitive and communication abilities
4. Evaluation of nutritional status and bone health
5. Consultation with rehabilitation team and other specialists
Postoperative Rehabilitation
1. Pain management
2. Physical therapy to maintain range of motion and strength
3. Occupational therapy to improve daily functioning
4. Orthotics and assistive devices to support mobility and balance
5. Regular follow-up with orthopedic surgeon and rehabilitation team
Outcomes and Research
1. Improved mobility and function
2. Reduced pain and discomfort
3. Enhanced quality of life
4. Prevention of deformities and complications
5. Ongoing research focuses on optimizing surgical techniques, improving outcomes, and reducing complications.
